Before sunrise, a small-town pharmacist unlocks her doors. She already knows who’s stretching insulin, who’s working double shifts while caring for an aging parent, and which neighbor depends on today’s refill to keep working tomorrow.
Her quiet presence holds that town together more than any headline ever could.
That same ethic — trust, responsibility, and service — is what Alabama’s rural health system needs now.
At this point, the question isn’t whether the Alabama Rural Health Transformation Program looks good on paper. It’s whether it can take root in Alabama soil.
That soil is shaped by distance and grit, by families who look out for one another, and by the uneven progress that comes when every county’s story is a little different.
We’ve talked about transparency, accountability, and sustainability. Now it’s time to talk about trust; the piece that ties it all together.
These aren’t slogans. They’re habits of systems that last.
Trust is harder to measure and easier to lose. Rural counties across Alabama face shortages in nurses, primary care, behavioral health, and emergency services. Hospitals run on margins so thin that one delay in reimbursement can break them.
Broadband gaps limit telehealth. Roads and bridges age faster than they’re repaired. Folks have seen programs come and go, each with a promise that faded when priorities changed. These aren’t excuses to stop; they’re reminders to move wisely, and with both feet on the ground.
Local innovation doesn’t mean winging it. It means deliberate design that fits each community’s rhythm; design that improves access, quality, and workforce stability.
But innovation needs breathing room. Rural clinicians spend too much time buried in paperwork, tangled data systems, and reimbursement hurdles that sap energy.
The friction isn’t from a lack of care; it’s from the weight of a system too complicated for its own good.
If we want local innovation to thrive, communities need help navigating regulations, using data well, and securing steady funding that rewards results.
Reimbursement must be reliable so clinics can plan, retain staff, and invest in better care. And the pace of change must match what rural areas can realistically absorb because progress that outruns people leaves them behind.
When those conditions line up, progress becomes more than a plan. It becomes practice.
Picture a rural hospital working with a farm co-op to bring screenings into the fields and poultry houses, checking blood pressure and talking nutrition during lunch breaks.
Picture a pharmacy partnering with a church to organize volunteer drivers so older neighbors can make their appointments. Imagine a manufacturing plant setting up a small telehealth room after shifts because a healthy workforce is good for business.
These aren’t daydreams. They’re the kind of local solutions that can bloom when state partnership meets community ingenuity.
But too often, good ideas stall. Overlapping regulations blur authority. Reporting requirements multiply faster than results. Priorities shift with politics, and communities are left holding the bag. Rural Alabama doesn’t resist change; it resists being changed without trust.
That’s where our leaders come in. Alabama can reduce that friction by pairing flexibility with fairness and freedom with a little common-sense oversight.
At the center of that balance is trust.
Rural communities remember who shows up and who disappears after the funding dries up. Long-term success depends on leaders who stay present, who listen before deciding, and who let local voices shape the work. Trust grows when nurses, pharmacists, and emergency crews know their effort is seen and supported.
The small-town pharmacist doesn’t open her doors because a policy manual tells her to.
She does it because her neighbors count on her.
The same spirit moves pastors who host screenings, teachers who connect families to care, and employers who make space for telehealth so workers can stay healthy and productive. Honoring that ethic means building a system that grows with the people it serves.
Key Takeaways for Leaders:
- Back local ideas first. Communities know what works best; give them room and resources to lead.
- Trust is everything. Show up, listen closely, and follow through.
- Treat schools, churches, employers, and nonprofits as part of health care. They extend access and strengthen resilience.
- Allow flexibility but measure results. Try new approaches, track what works, and stop what doesn’t.
- Make funding predictable and long-term. Uncertain money means uncertain care.
- Cut paperwork and simplify payments. Let clinicians care instead of wrestle bureaucracy.
- Provide technical support for data, regulations, and funding so ideas can take root and grow.
- Value steady presence over big launches. Small, consistent actions build systems that last.
Real transformation won’t come in a burst of fanfare or a single initiative. It’ll come the way it always has in rural Alabama: through steady presence, quiet persistence, and a shared belief that our neighbors’ wellbeing is worth the effort.
If Alabama wants a rural health system that endures, our leaders must match that steadiness. Communities will be watching for follow-through when funding decisions come due, and for consistency across agencies and election cycles. Trust grows when words become habits and commitments turn into practice.
Alabama doesn’t need a dramatic gesture. It needs leadership that stays put, empowers local problem-solving, and protects the partnerships already holding our towns together. That’s how fragile systems become resilient ones. And how Alabama keeps its promise to the people who keep the lights on long before the day’s first shift begins.
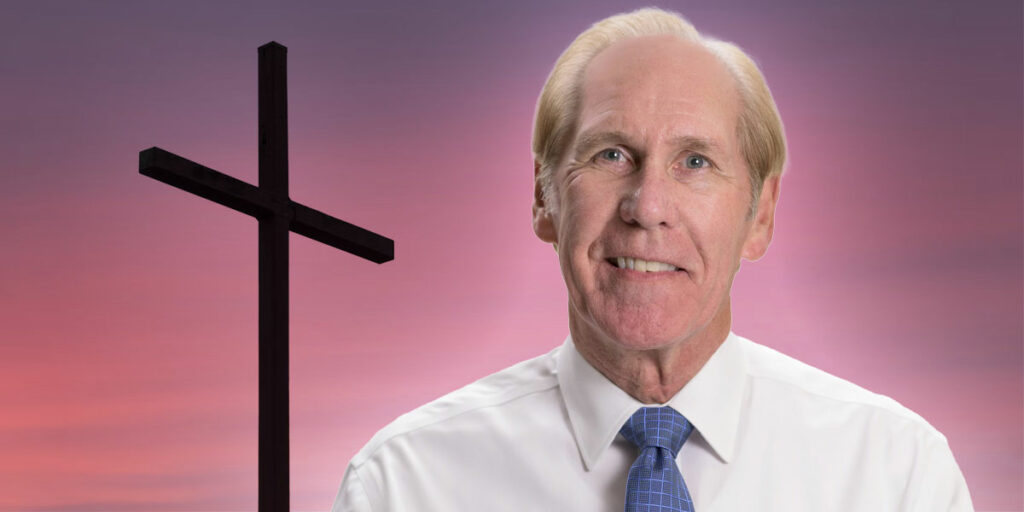
David L. Albright, PhD, is a University Distinguished Professor at The University of Alabama, a board member of the DCH Healthcare Authority, and immediate past president of the Alabama Rural Health Association. The views expressed here are his own and do not necessarily reflect those of his institution or any affiliated organizations.