Why is the COVID-19 virus more dangerous in people with existing illnesses?
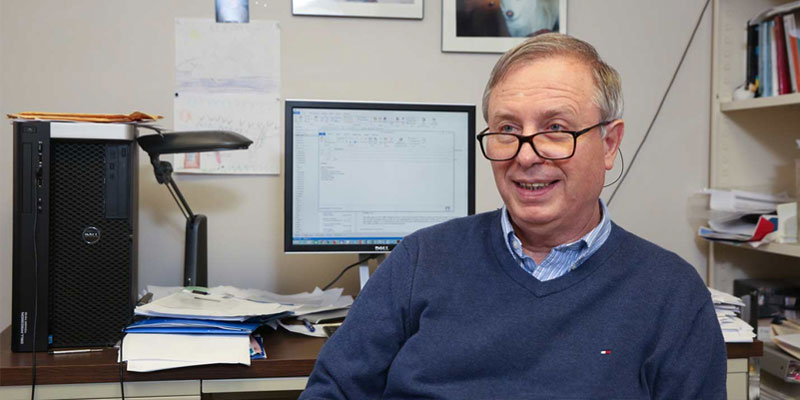
Sadis Matalon, of the University of Alabama at Birmingham, and colleagues in Texas and San Francisco asked that question in a hypothesis paper published online in Physiological Reviews on March 27. They reviewed, in detail, research literature for hypertension, diabetes, coronary heart disease, cerebrovascular illness, chronic obstructive pulmonary disease and kidney dysfunction, as well as many viral studies, studies of COVID-19 pathology and clinical presentation, and literature on the life-threatening acute respiratory distress syndrome.
Twelve days later, UAB Professor Emeritus Timothy Ness posted plans on ClinicalTrials.gov for an exploratory COVID-19 outpatient study to test Matalon’s hypothesis and prevent worse clinical outcomes. His quick reaction is another example of how nimble UAB researchers have been during the COVID-19 pandemic.
In the Physiological Reviews paper, the researchers noted that all those comorbidities feature elevated levels of the extracellular protease plasmin. Plasmin is able to nick proteins at amino acid sequences called furin sites. For many viruses, this nicking increases their infectivity. Both SARS and MERS – the two virulent coronaviruses that are related to the COVID-19 virus – “have evolved an unusual two-step furin activation for fusion, suggestive of a role during the process of emergence into the human population,” the researchers wrote.
They noted that the COVID-19 virus, SARS-CoV-2, has a furin site on its spike protein, the vital protein for viral attachment to a lung cell. The researchers proposed that plasmin may cleave that site in the spike protein to increase its infectivity and virulence, and they hypothesized that, “the plasmin system may prove a promising therapeutic target for combating COVID-19.”
Ness already knew there is an inexpensive, commonly used drug – tranexamic acid, or TXA – that targets plasmin by inhibiting its conversion from the inactive precursor, plasminogen, to the active protease, plasmin.
TXA is approved by the U.S. Food and Drug Administration for treatment of heavy menstrual bleeding because having lower plasmin levels allows better clotting. TXA has a long track record of safety and is commonly given off-label. At UAB Hospital, TXA is used as a standard of care for orthopedic and cardiac bypass surgeries; it is commonly used for hemorrhaging trauma patients and has been used for spinal surgery, neurosurgery and corrective jaw surgeries. It is being studied for use in cesarean section surgeries.
For the clinical trial, Ness and colleagues have started a double-blind study, giving either TXA or a placebo pill to COVID-19 outpatients who were recently diagnosed. Patients also receive an anticoagulant. The overall goal of the exploratory study is to assess the safety and efficacy of five days of TXA versus placebo. Enrollment is ongoing.
Ness and colleagues hypothesize that the TXA treatment will reduce the infectivity and virulence of the virus, as measured by reduced need for hospitalization within a week if a patient’s condition deteriorates. Adults 19 years old and older are eligible, and all patients – whether in the control group or the TXA group – receive standard care as directed by their primary caretakers.
To learn more about the study, “TXA and Corona Virus 2019 (COVID19) in Outpatients,” patients and physicians can contact Dr. Timothy Ness at [email protected]. Patients who have recently tested positive for COVID-19 can call 205-934-6777 to see if they qualify for the study.
Other principal investigators for the trial are Dr. Sonya Heath, professor in the UAB Department of Medicine Division of Infectious Diseases; Dr. Brant Wagener, associate professor and Sadis Matalon, distinguished professor, both in the UAB Department of Anesthesiology and Perioperative Medicine. Ness is professor emeritus in that department.
Authors of the Physiological Reviews paper, “Elevated plasmin(ogen) as a common risk factor for COVID-19 susceptibility,” are Hong-Long Ji and Runzhen Zhao, University of Texas Health Science Centre at Tyler; Michael A. Matthay, University of California, San Francisco; and Matalon.
Matalon said the paper has been widely noticed. “Since its publication online, it has been downloaded 26,565 times and cited 55 times,” he said.
At UAB, Matalon holds the Dr. Alice McNeal Endowed Chair in Anesthesiology, and he is a Distinguished Professor and vice chair for Research.
(Courtesy of Alabama NewsCenter)